Katherine Wells still remembers finding out that measles had hit West Texas.
It was late January, and Wells, the director of the Lubbock Health Department, was notified that a child from nearby Gaines County was being treated for the respiratory disease at one of the local hospitals in Lubbock County.
At that point Lubbock County had not recorded a measles case in more than 20 years. Neither Wells nor her staff had seen measles in their careers.
“I started talking to people from Gaines County and realized that there were a lot of sick people on the ground, that measles was already spreading,” she said. “So it was that moment where we realized that this was much bigger than one measles case.”
Gaines County was the epicenter of an outbreak that is still spreading around the United States. As of July 15, there have been 1,309 confirmed measles cases around the country this year, the highest number of cases in more than 30 years. Most cases in 2025 are among unvaccinated children.
The bulk of the measles cases this year have been in Texas, which to date includes more than 760 confirmed cases. More than half have been in Gaines County.
While Lubbock County has reported just over 50 measles cases, it’s intertwined with Gaines County due to their close proximity. Gaines County has a small hospital, so children hospitalized for measles were typically transferred to Lubbock County’s free-standing children’s hospital or another hospital with a children’s unit, according to Wells.
Wells has seen this outbreak up close, and her experiences trying to stop measles in her county — which Texas removed recently from its list of active outbreaks, along with Gaines County — hold lessons for other communities. She hopes some of her department’s work in mitigating the spread can be a blueprint for public health officials elsewhere who are now recording their first cases.
Still, Wells also worries about how expected federal funding cuts could impact her efforts to keep Lubbock County residents protected from future outbreaks.
“It’s so important that we have local people on the ground that understand our communities, that can respond to these things — and I do worry that the ability to continue to do that work is at risk with some of the federal cuts we’re seeing to money that flows down to local public health,” she said.
With six months left in the year, public health officials and experts say it’s hard to predict how this outbreak, which consists of cases in more than 35 states, will evolve. Measles was declared eliminated from the United States in 2000, due in part to widespread vaccination. Researchers believe the United States, like some other countries with increasing cases, could soon lose its status.
While the number of reported cases has slowed in recent months, upcoming back-to-school activities in the fall typically bring together large groups of children. Measles, which is not a seasonal disease, is highly contagious and spreads when an infected person breathes, coughs or sneezes.
The outbreak comes at a time of heightened distrust in government officials and a proliferation of disinformation and misinformation online about vaccines. And amid proposed federal budget reductions, Health and Human Services Secretary Robert F. Kennedy Jr. has mischaracterized the safety of the highly effective measles-mumps-rubella (MMR) vaccine.
Those dynamics, along with declining vaccination rates, spell new challenges for public health officials.
“I think local public health department directors have an uphill battle — responding to measles and trying to get people vaccinated with a vaccine that we’ve had for over 50 years. You’d hope people would trust and believe that that’s what we need to do,” Wells said. “It’s going to be a challenge for public health officials to get those messages out to the right individuals.”
At the height of the measles outbreak in late winter and early spring, the days were long for Wells, who said she worked seven days a week. She coordinated lab testing to confirm cases. She organized contact tracing to help stop the spread. She spoke to the public through news releases and the press about the ebbs and flows of the disease. She watched as national attention heightened with the deaths of two children. With no new dollars, Wells said she offered comp time to eligible staff to address the extra hours they were working.
“I think measles felt worse than COVID, and suddenly it brought back some of the trauma that we went through with COVID,” she said.
Wells has some advice for other public health officials who are now just starting to see their first cases: Reach out to community stakeholders and make a plan. That means being in contact with school superintendents, camp directors and day care staff — any place where children gather.
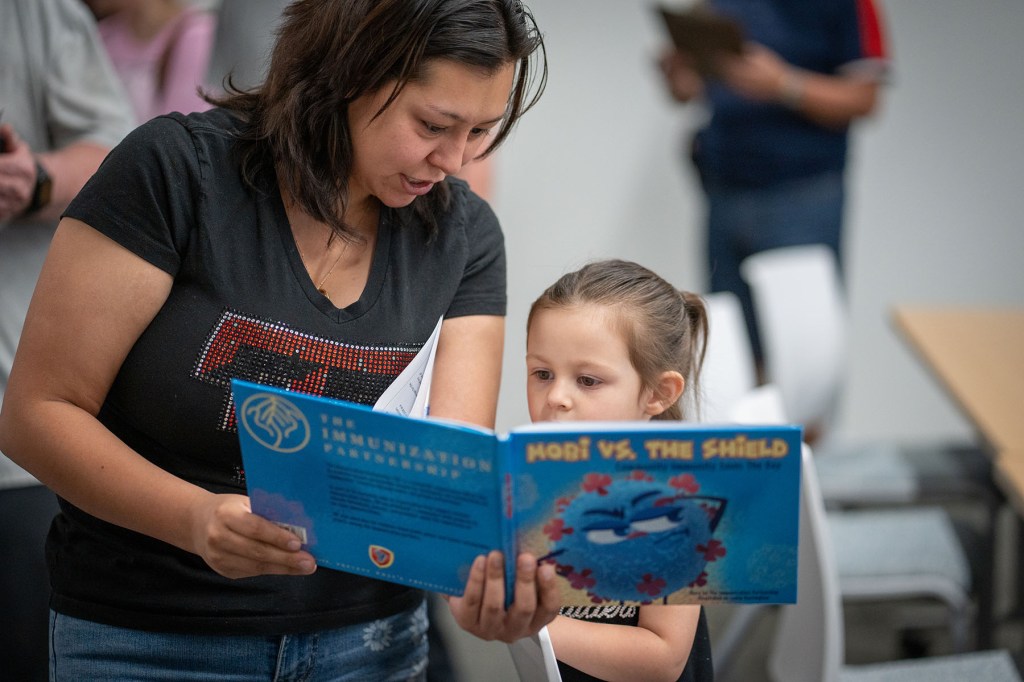
(Jan Sonnenmair/Getty Images)
“Make sure that you have those relationships in case measles enters one of those settings,” she said.
Wells also recommended that public health officials look at geographical data to try to figure out where there are pockets of low vaccination rates to reach out to those potentially skeptical communities.
“Where you see low vaccination rates, engage with them and talk to them about measles and how we’ve hit this 30-year high, and is there anything that the public health department can do to support those groups getting vaccinated?” she said.
Chrissie Juliano is the executive director of the Big Cities Health Coalition (BCHC), an organization that represents the country’s largest metropolitan health departments, which cover about 61 million people. She said federal funding cuts — those being challenged via litigation and proposed cuts in future budgets — will make it more difficult for local public health departments to respond to measles and other infectious diseases. The federal government has been central to funding a lot of public health. More than 70 percent of the Centers for Disease Control and Prevention’s domestic budget goes to state and local communities.
Wells said she expects her department’s budget to be impacted, as news reports indicate at least $100 million in federal dollars will not be available again for Texas public health departments to use on disease detection and prevention efforts.
“I don’t know exactly what will be impacted, but I’m planning for cuts to our department,” she added.
In Dallas County, Texas, just a few hundred miles from Gaines and Lubbock counties, officials said they cancelled vaccine clinics to administer MMR vaccines because federal dollars had been rescinded.
“This was a really specific impact of a local health department trying to be proactive, to use the data, make decisions, reach out to the community to fill a gap among people who needed vaccines — and then could not because of resources taken away,” Juliano said.
The impact of federal funding cuts is popping up elsewhere. In Minneapolis, public health officials announced in March that they had halted their vaccination program, which included administering vaccines to young children. In Columbus, Ohio, public health officials laid off 11 employees in April, many of whom were infectious disease specialists.
Kennedy has defended proposed HHS budget cuts by claiming that critical staff have not been cut and other key programs will be consolidated.
Adam Ratner is a pediatric infectious diseases physician who treated children with measles during the outbreak in New York. He used that experience to write: “Booster Shots: The Urgent Lessons of Measles and the Uncertain Future of Children’s Health.”
Ratner noted that it took almost 40 years after a measles vaccine was developed to reach the eradication status that the United States reached in 2000. During that time, public health officials and policy makers worked toward supporting school vaccine mandates and making vaccines more accessible, especially to families of low-income children.
Ratner worries that Kennedy’s messaging on vaccines — which has included spreading disinformation about one of the two children who died earlier this year from measles — could preview more limited federal resources to combat the spread of disease. Kennedy sent some temporary personnel from the Centers for Disease Control and Prevention to West Texas at the height of its outbreak.
“We’re in a situation where the priorities from HHS and just generally in terms of federal funding for public health are to decrease funding, decrease emphasis on vaccination, and that’s a very dangerous situation,” he said.
In Lubbock County, Wells said the federal government and state health department brought in some additional temporary staff at the height of the outbreak, noting the CDC personnel. But she added that these contractors typically had to work 40 hours a week. Without new dollars in her department’s coffers, she was limited in her financial flexibility as a public health official to build the very trust experts say is needed right now.
“I would have preferred to bring in local nurses that would have been happy with very flexible hours to be administering the vaccine — ‘I’m a retired school nurse, and I’m giving you this vaccine’ is much better than having a nurse coming in from outside of our community,” she said. “I just think it brings that trust factor in.”
While the end of measles cases in Lubbock and Gaines counties were marked unceremoniously when the locations were removed from a state website with active areas, Wells just took her first real vacation of the year.
“I took a real week off, stepping away from work,” she said. “I’m also requiring all of my managers that worked through all of this to take some time off.”
Wells said measles can easily reemerge in Lubbock. This time, she feels more equipped. She has her staff ready for surveillance. She now has a local public health laboratory for the region to test more quickly for measles. All the providers are well aware of measles protocols to help stop transmission. She is staying vigilant — while also planning for potential federal funding cuts to her department.
“We’re such a mobile society that it would just take one unvaccinated person to drive to another area of the state or the country that has a measles outbreak and bring it back into Lubbock,” she said.
Great Job Barbara Rodriguez & the Team @ The 19th Source link for sharing this story.