This analysis was originally published by KFF Health News, a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—the independent source for health policy research, polling and journalism.
Affordable Care Act (ACA) enhanced premium tax credits are set to expire at the end of this year. Enhanced premium tax credits were introduced in 2021 and later extended through the end of 2025 by the Inflation Reduction Act. The enhanced tax credits both increased the amount of financial assistance already eligible ACA Marketplace enrollees received as well as made middle-income enrollees with income above 400 percent of federal poverty guidelines newly eligible for premium tax credits.
Since the introduction of the enhanced premium tax credits, enrollment in the Marketplace has more than doubled—from about 11 to over 24 million people, the vast majority of whom receive an enhanced premium tax credit. If enhanced tax credits expire, many Marketplace enrollees will continue to qualify for a smaller tax credit, while others will lose eligibility altogether and be hit by a “double whammy” of losing their entire tax credit and being on the hook for rising premiums.
Since 2014, the ACA has capped how much subsidized enrollees pay for their health insurance premiums at a certain percent of their income, on a sliding scale, with the federal government covering the remainder in the form of a tax credit. Enhanced tax credits work by further lowering the share of income ACA Marketplace enrollees pay for a plan.
For example, with the enhanced tax credits in place, an individual making $28,000 will pay no more than around 1 percent ($325) of their annual income towards a benchmark plan. If the enhanced tax credits expire, this same individual would pay nearly 6 percent of their income ($1,562 annually) towards a benchmark plan in 2026. In other words, if the enhanced tax credits expire, this individual would experience an increase of $1,238 in their annual premium payments net of the tax credit.

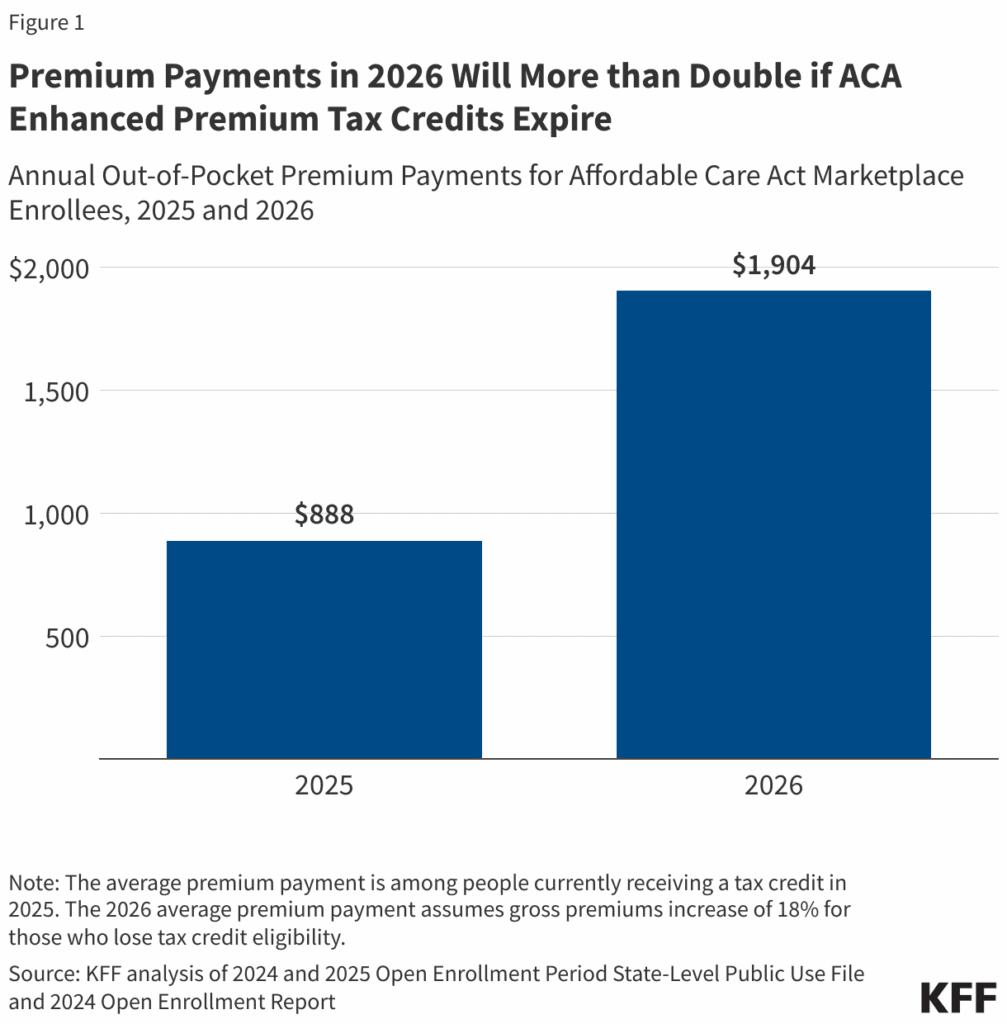
A previous KFF analysis, based on data released by the federal government, showed the enhanced premium tax credits saved subsidized enrollees an average of $705 annually in 2024, bringing their annual premium payment down to $888. Without the enhanced premium tax credits, annual premium payments in 2024 would have averaged $1,593 (over 75 percent higher than the actual $888). More recent data have not been released.
Based on the earlier federal data and more recent other publicly available information, KFF now estimates that, if Congress extends enhanced premium tax credits, subsidized enrollees would save $1,016 in premium payments over the year in 2026 on average. In other words, expiration of the enhanced premium tax credits is estimated to more than double what subsidized enrollees currently pay annually for premiums—a 114 percent increase from an average of $888 in 2025 to $1,904 in 2026. (The average premium payment net of tax credits among subsidized enrollees held steady at $888 annually in 2024 and 2025 due to the enhanced premium tax credits).
The increase in premium payments with expiration of the enhanced premium tax credits is even higher than previously estimated for two reasons:
- Trump administration changes to tax credit calculations, and
- Rising 2026 premiums.
The Trump administration made changes to the way tax credits are calculated, which were finalized in the ACA Marketplace Integrity and Affordability rule. The required contribution levels that will be in place for 2026 if the enhanced tax credits are not renewed will be higher relative to the required contribution levels calculated under the original methodology based on rules in effect at the time. This means that enrollees are expected to pay a higher share of their income towards a benchmark premium plan in 2026 than they otherwise would have. Additionally, inflation in private insurance premiums has led to higher premium contribution levels than previously expected.
Additionally, insurers in the ACA Marketplace are proposing to raise their rates by a median of 18 percent. Fueled by rising health care costs and the expiration of the enhanced premium tax credits, insurers are proposing the largest rate increases in 2026 since 2018, the last time uncertainty over federal policy changes contributed to sharp premium increases. As premiums increase, the enhanced tax credits provide additional savings to enrollees that receive them. This means that middle-income enrollees, whose payment for a benchmark plan is currently capped at 8.5 percent of their income and will lose financial assistance altogether, will have to cover the cost of premium increases in addition to the amount their tax credits would have previously covered to keep their same plan.
Enrollees Across the Income Spectrum Can Expect Big Increases in Premium Payments
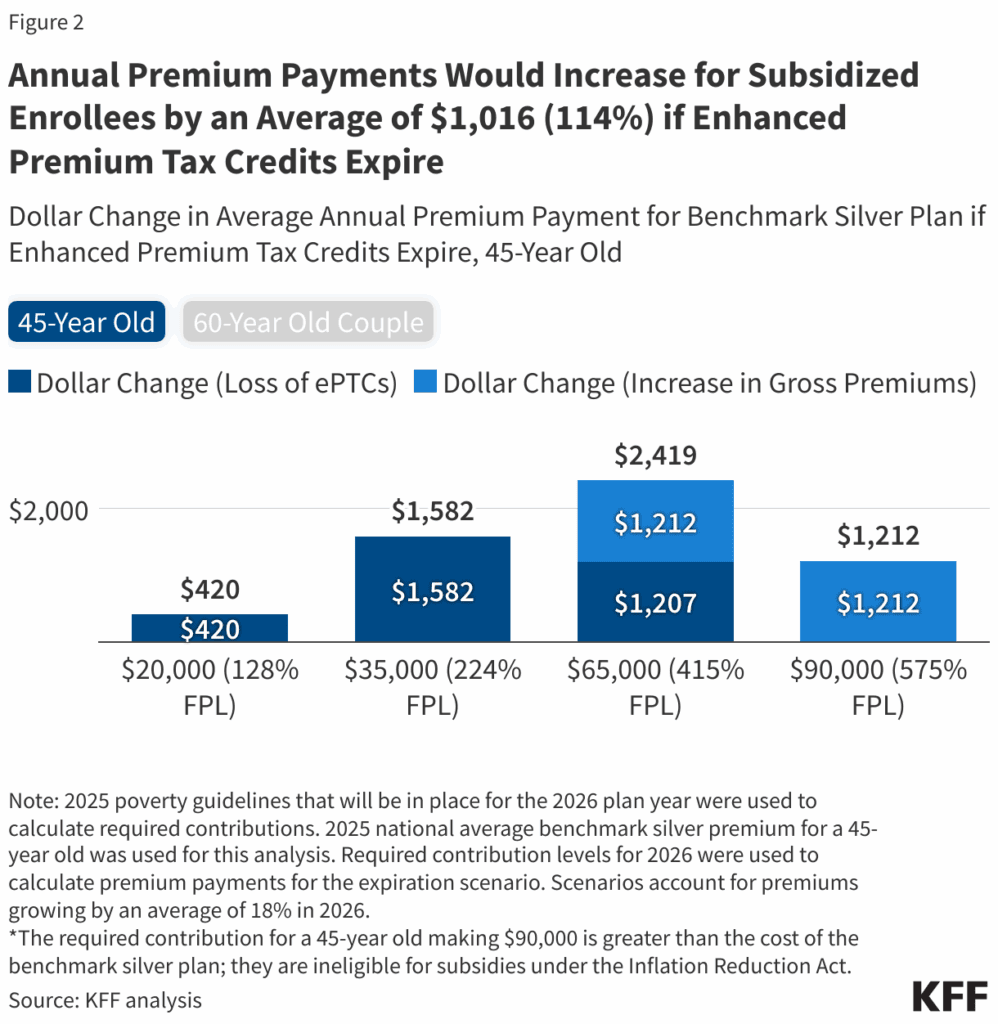
Enrollees with incomes above 400 percent of poverty will be subject to large increases in premium payments if enhanced premium tax credits expire. On average, a 60-year-old couple making $85,000 (or 402 percent FPL) would see yearly premium payments rise by over $22,600 in 2026, after accounting for an annual premium increase of 18 percent. This would bring the cost of a benchmark plan to about a quarter of this couple’s annual income, up from 8.5 percent. Meanwhile, a 45-year-old earning $20,000 (or 128 percent FPL) in a non-Medicaid expansion state would see their premium payments for a benchmark plan rise from $0 to $420 per year, on average, from the loss of enhanced premium tax credits. About half (45 percent) of ACA Marketplace enrollees have incomes between 100-150 percent of poverty, about a fourth (28 percent) have incomes between 150-250 percent of poverty, and roughly 1 in 10 have incomes above 400 percent of poverty.
Justin Lo is a senior researcher for the Program on Patient and Consumer Protections and the Program on the ACA. In this role, he focuses on the impact of health policy on patients’ experience with health care and marketplace insurance. Prior to joining KFF, he worked at Epic Systems, where he supported health systems in achieving their population health management objectives and conducted clinical epidemiologic studies using electronic health records.
Larry Levitt is the executive vice president for health policy, overseeing KFF’s policy work on Medicare, Medicaid, the healthcare marketplace, the Affordable Care Act, racial equity, women’s health and global health.
Jared Ortaliza is a policy analyst at KFF for the Program on the ACA, where he analyzes economic and policy research on the ACA Marketplaces, including Marketplace enrollment, costs and affordability. Prior to joining KFF, he was an outbreak investigator for the Los Angeles County Department of Public Health. Jared graduated from University of California, Los Angeles with a B.S. in Human Biology and Society.
Cynthia Cox is a vice president and director of the Program on the ACA, where she conducts economic and policy research on the Affordable Care Act and its effects on private insurers and enrollees. Her work focuses on enrollment, pricing and competition in the ACA’s exchange markets. Cox also directs the Peterson-KFF Health System Tracker, a partnership of the Peterson Center on Healthcare and KFF aimed at monitoring the performance of the U.S. health system over time and in relation to other large, high-income countries. Her work on this project focuses on trends in health care costs, access and affordability, as well as measures of health care quality and outcomes.
Great Job Justin Lo & the Team @ Ms. Magazine Source link for sharing this story.



